ABSTRACT
Objective: The inflammatory response after cardiac surgery increases vascular permeability leading to higher mortality and morbidity in the post operative time. The modified ultrafiltration (MUF) had shown benefits on respiratory, and hemodynamic in pediatric patients. This approach in adults is not well established yet. We hypothesize that modified ultrafiltration may improve respiratory, hemodynamic and coagulation function in adults after cardiac surgeries. Methods: A prospective randomized study was carried out with 37 patients who underwent coronary artery bypass graft surgery (CABG) were randomized either to MUF (n=20) at the end of bypass or to control (no MUF) (n=17). The anesthesia and ICU team were blinded for the group selection. The MUF were carried out for 15 minutes after the end of bypass. The patients data were taken at beginning of anesthesia, ending of bypass, ending MUF, 24 hours, and 48 hours after surgery. For clinical outcome the pulmonary, hemodynamic and coagulation function were evaluated. Results: We observed lower drain loss in the MUF group compared to control group after 48 hours (598 ± 123 ml vs. 848 ± 455 ml; P=0.04) and required less red blood cells units transfusion compared to control group (0.6 ± 0.6 units/patient vs.1.6 ± 1.1 units/patient; P=0.03). The MUF group showed lower airway resistance (9.3 ± 0.4 cmH2O.L-1s-1 vs. 12.1 ± 0.8 cmH2O.L-1s-1; P=0.04). There were no deaths in both groups. Conclusion: The MUF reduces post operatory bleeding and red blood cells units transfusion, but with no differences on clinical outcome were observed. The routinely MUF employment was not associated with hemodynamic instability.
RESUMO
Introdução: A cirurgia cardíaca com circulação extracorpórea aumenta a permeabilidade vascular, com incremento da morbidade e da mortalidade pós-operatória. A ultrafiltração modificada na população pediátrica demonstrou melhora da função pulmonar e hemodinâmica, contudo benefício semelhante não está bem estabelecido em adultos. Nós temos a hipótese que a ultrafiltração modificada pode melhorar a função pulmonar, hemodinâmica e a coagulação no pós-operatório em pacientes adultos. Métodos: Estudo prospectivo e cego para a equipe anestésica e da terapia intensiva em pacientes eletivos submetidos à revascularização do miocárdio. Todos os pacientes foram monitorados quanto à função hemodinâmica, pulmonar e hematológica no intraoperatório e até 48 horas de pós-operatório. Os pacientes foram divididos em dois grupos: um submetido à ultrafiltração modificada por 15 minutos após a saída de circulação extracorpórea e um grupo sem ser submetido à ultrafiltração. Os dados foram estudados com análise de variância com dois fatores para medidas repetidas. Resultados: O grupo ultrafiltração modificada apresentou menor sangramento pós-operatório ao final de 48 horas (598 ± 123 ml vs. 848 ± 455 ml; P = 0,04) e menor necessidade de transfusão de unidades de hemácias (0,6 ± 0,6 unidades/paciente vs. 1,6 ± 1,1 unidades/paciente; P =0,03). O grupo ultrafiltração apresentou menor resistência de vias aéreas quando comparado ao controle (9,3 ± 0,4 vs. 12,1 ± 0,8 cmH2O. L-1s-1; P =0,04) e menor complacência quando comparado ao controle (47,3 ± 2,0 mLcmH2O vs. 53,1 ± 3,1 mLcmH2O; P=0,04). Conclusão: O uso ultrafiltração modificada diminuiu o sangramento pós-operatório e a necessidade de transfusão, contudo sem diferenças no resultado clínico final. O uso da ultrafiltração modificada não foi associado com instabilidade hemodinâmica.
INTRODUCTION
The application of extracorporeal circulation (ECC) in heart surgeries triggers a systemic inflammatory reaction that may contribute to the increase of postoperative mortality and morbidity [1-3]. The clinical inflammatory response manifests by means of increase in vascular permeability, interstitial edema and decline in the respiratory and cardiovascular function. Several strategies have been described in the attempt of minimizing the inflammatory response, such as minimally invasive surgeries [4], anti-inflammatory drugs [5,6] and hemofiltration during surgery. The latter modality, more specifically, the modified ultrafiltration, was describer by Elliot et al. [7] and initially used in pediatric patients.
The modified ultrafiltration is performed after the end of ECC and presents its benefits well documented in pediatric patients with improvement in the pulmonary and hemodynamic function, reduced need of red blood cell unit transfusions and lower drain loss in the postoperative [5, 8-11]. However, the application of modified ultrafiltration in adults is not well studied regarding its effects in coagulation, pulmonary and hemodynamic function. There are not many reports concerning its safety and efficiency, and whether the benefits described in children also occur in adults [12]. The present work was performed in order to analyze the effects of MUF in the respiratory and cardiovascular function, need of hemoderivative transfusion and postoperative drain loss inelective coronary artery bypass graft surgery.
METHODS
Patient selection
After approval of the Ethics in Research Committee of our institution and registration in the National Ethics in Research System the patients were included in a prospective, randomized and blind study to the anesthesia and ICU team. The included patients presented the following characteristics: male/female, coronary artery bypass graft surgery, ejection fraction higher than 40%, which was estimated by cardiac catheterism in anterior right oblique projection, elective surgery, diabetics or non-diabetics. The criteria of exclusion were: presence of any kind of neoplasia, depressed renal function that was defined as creatinine clearance lower than 45ml/minute for males and lower than 40ml/minute for females.
Surgical procedure
The patients were submitted to inhalant and endovenous balanced anesthesia that was decided by the anesthetist, who was blind to the type of treatment from the beginning of surgery until the end of ECC when the treatment was applied. The patients were submitted to median sternotomy mediana, cannulation of the ascending aorta and right atrium with double-phase cannula. The types of grafting and places were discussed previously and agreeably with the patient's cardiologist. The patients were submitted to extracorporeal circulation with adult membrane oxygenator (Braile Biomédica, São José do Rio Preto, Brazil), nasopharyngeal temperature of 32ºC, tepid anterograde blood cardioplegia.
The distal anastomoses were performed with clamping aorta. After performing the distal anastomoses, the aorta was unclamped. Afterwards the aorta was clamped laterally in order to perform the proximal anastomoses in the ascending aorta. At end of all anastomoses, the patient was removed from extracorporeal circulation and after 15 minutes of stabilization the patients were randomized to either study or control group. The modified ultrafiltration group (MUF) was submitted to ultrafiltration by aspirating the blood from the ascending aorta by cardioplegic cannula with flow of 300ml/m during 15 minutes. The blood originating from the cardioplegic cannula ran through the hemoconcentrator H-500 (Braile Biomédica, São José do Rio Preto, Brazil), where it was heated at 38ºC, then hemoconcentrated and finally returned by the venous line to the right atrium. The arterial cannula was kept for the infusion of the remaining volume in the reservoir (Figure 1). The Control Group was not submitted to MUF and only observed during 15 minutes and received the remaining volume of the oxygenator. The hemoconcentrator H-500 possesses fibers of polyethersulfon and the size of the pores is 20 kDaltons.
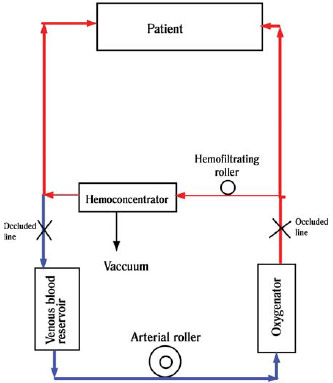
Fig. 1 - Scheme of modified ultrafiltration. Notice the fact that the patient is off extracorporeal circulation. The blood is aspirated from the aorta, runs through the hemoconcentrator and returns by the venous line of the patient
At the end of MUF or observation, the hemostasia was reviewed and the patient was closed in the conventional manner and referred to the intensive care unit.
Respiratory monitoring, hemodynamic and regime of data and samples collection
All patients after anesthetic induction were monitored by Swan-Ganz continuous debit catheter (Edwards Lifesciences, Irvine, USA), invasive blood pressure in the left radial artery and the orotracheal tube was connected to the device Co2smo Plus DX 8100 (Dixtal/Novametrix, Wallingford, USA). The patients had their respiratory and hemodynamic data filed and blood samples collected in the following periods: anesthetic induction, 15 minutes after discontinuing ECC and immediately preceding MUF, immediately following MUF, 24 hours of postoperative and 48 hours of postoperative.
The cardiac debit, systemic vascular resistance and pulmonary vascular resistance were normalized in the body surface. The oxygen drainage (DO2), oxygen consumption (VO2), oxygen extraction (EO2), pulmonary shunt (Qs/Qt), alveolus-arterial difference (Aa-difference) and oxygenation index were calculated as previously described [13].
The airways resistance and pulmonary compliance were acquired by the data provided by the device Co2smo Plus DX 8100, which was performed in a continuous manner by the equipment. The hematocryt, serum lactate dosage, platelet counting, white blood cell counting, creatinine dosage, activated partial thromboplastin time (R) and international normalized ratio of prothrombin time (INR) were acquired from the results of the main laboratory of our institution.
The data relating to bleeding, amount of fresh frozen plasma and concentration of erythrocytes transfused per patient were filed from the intensive care unit report. Negative events such as death, cerebrovascular accident, reoperation and perioperative infarction were filed. The perioperative infarction was defined as the appearance of new Q waves in the electrocardiogram of twelve conventional derivations.
The intensive care unit team was blind for the patients group selection, the decisions regarding transfusion and postoperative management were not made by the surgical team. As a protocol of the institution, the patients must receive transfusion if the hematocryt is lower than 28 % and fresh frozen plasma transfusion if there is NIR higher than 2 and/or R higher than 2, however, the final decision has always been made by the physician in the intensive care unit.
Statistical analysis
The continuous variables were expressed as mean and standard deviation, and the categorical variables were expressed as usual. All variables were tested for normality and the necessary changes were used when required. The size of the sample was estimated with pilot test using three patients considering alpha of 0.05, beta of 0.8 and a minimal difference in the hemodynamic variables of 10%. The reason for the choice of the hemodynamic variables was due to the minimal variability found in the pilot test. It was used the software G*Power version 3 for Macintosh (Institute of Psychology, Düsseldorf, Germany).
For the analysis of the means it was used the Student's t test for non-parallel samples. The categorical variables were analyzed with the chi-square test.
For the analysis between the groups and in different times it was applied variance analysis with two factors for repeated measures (Two-way ANOVA) and the post-test of Bonferroni to determine when possible where the differences occurred. The differences were considered significant with
P < 0.05. It was applied the statistical package GraphPad version 5.0 for Macintosh (Graphad Software, California, USA).
RESULTS/DISCUSSION
Cardiac surgery is associated with the increase of vascular permeability, liquid retention causing an increase in postoperative mortality and morbidity [14]. Methods that are capable of minimizing this response are constantly reported in literature [1,2]. In the present study we have shown that the modified ultrafiltration was not associated with negative events such as hemodynamic instability or decline in pulmonary function showing that its application was safe. In addition to its safe application, modified ultrafiltration provided decrease in the airways resistance, less postoperative bleeding and less need for transfusion when compared to the control group. Nevertheless, these differences in the respiratory mechanics or bleeding did not produce better clinical results or shorter period of hospitalization (Table 1).

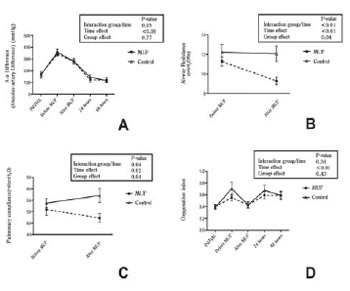
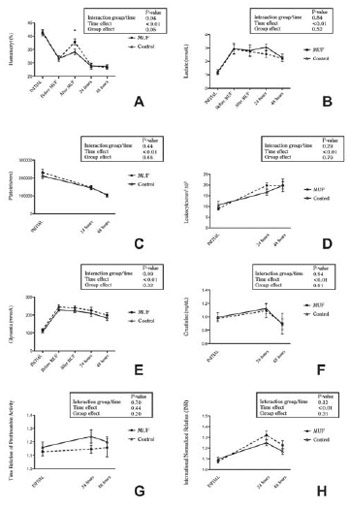
The importance of these findings is that MUF may diminish the need for hemotransfusion when applied routinely in adult patients. Our findings are consistent regarding the safety of application, as a result of the patients being monitored for hemodynamic, pulmonary and metabolic aspects, not presenting differences between both groups. The methodology applied to measure these variables proved to be adequate, for the means used are those routinely applied in clinical practice with enough accuracy and reliability (Figs 1 to 4).

Fig. 2 - Hemodynamic and oxygen conveyance variables. Analysis of variance with two factors for repeated measures. Values expressed in mean and two mean standard errors. (A) CI - cardiac index, (B) SVRi - systemic vascular resistance index, (C) PVRi - pulmonary vascular resistance index, (D) DO2 - oxygen drainage, (E) VO¬2 - oxygen consumption, (F) oxygen extraction
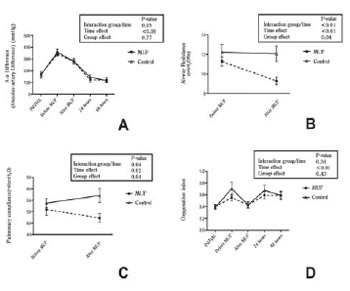
Fig. 3 - Respiratory mechanics variables and oxygenation index. Analysis of variance with two factors for repeated measures. Values expressed in mean and two mean standard errors. (A) alveolusarterial difference, (B) airways resistance, (C) pulmonary compliance, (D) oxygenation index
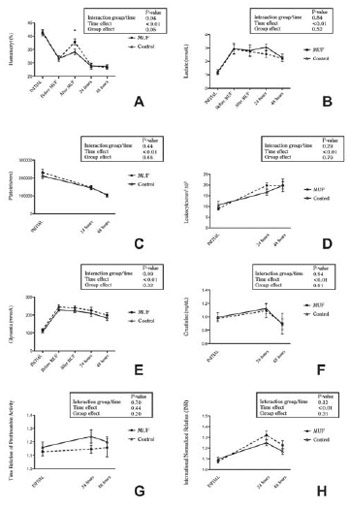
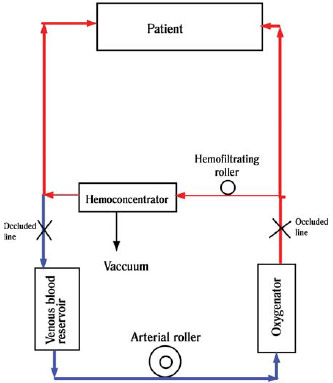
Fig. 4 - Hematimetric variables, leukocyte counting and coagulation. Analysis of variance with two factors for repeated measures. Values expressed in mean and two mean standard errors. (*) pre-MUF difference compared with post-MUF using the Bonferroni's post-test (P???0.05). (A) hematocryt, (B) serum lactate, (C) platelet counting, (D) leukocyte counting, (E) glycemia, (F) serum creatinine, time relation of de prothrombin activity (G), international normalized ratio
The basic difference between conventional ultrafiltration and MUF is that the first one can be performed during extracorporeal circulation and depends on the volume in the venous reservoir and what is effectively ultrafiltrated is the extracorporeal circulation system. MUF, on the other hand, is performed at the end of extracorporeal circulation with blood being directly aspirated from the aorta and then directed to the hemoconcentrator to be ultrafiltrated. After ultrafiltration in MUF, the blood returns by the venous line. In MUF what is effectively ultrafiltrated is the patient, for the ultrafiltration is performed out of extracorporeal circulation [7].
The MUF group showed values of drainage and consumption of oxygen very similar to those of the control group, we observed that these two variables behaved differently in both groups with decreased oxygen drainage to the end of 48 hours of postoperative and increase in oxygen consumption in the same period. This behavior has already been described by other authors in patients submitted to heart surgery [15] which only stresses the fact that MUF did not imply harmful implications in its application.
The MUF group showed decrease in airways resistance, decrease in compliance in the period immediately after its application when compared to the control group. Both parameters did not have clinical repercussion nor in the gas exchange variables such as oxygenation index or arterial-alveolar difference. The decrease in compliance observed in the MUF group cannot be explained solely by the treatment; a study similar to ours, in pediatric patients, could not establish any difference between the different types of treatment regarding compliance [16]. In another recent work, using ultrafiltration with zero balance during the entire surgical procedure, also in pediatric patients, showed decrease in pulmonary compliance and improve in the oxygenation index [17]. According to our knowledge in the reference literature, the present work is the first in adults that evaluated the pulmonary mechanics using MUF and a control group. Possibly the decrease in compliance in the MUF group is due to the brief period after the ultrafiltration procedure where the patients were more hemoconcentrated when compared to the control group, nonetheless, we do not have a more consistent explanation for this fact. Further studies must seek for other explanations for the fact.
A few works compared MUF in adults, Pérez-Vela et al., in 2008, compared the modified ultrafiltration with the conventional technique or the use of both in patients submitted to any type of heart surgery, he did not use a group without any type of treatment as control. The work shows findings very similar to ours, particularly, regarding less postoperative bleeding and respiratory variables. These findings also showed decrease in compliance in the group submitted exclusively to MUF which are very similar to those found in the present study [18]. In our work, we restricted the selection of our sample aiming to diminish factors that could complicate its interpretation and, likewise, we have achieved similar results as previously reported.
Although our study has shown less bleeding and less hematocryt concentration transfusion, it was not able to show any difference in the coagulation tests or platelet counting. We must observe that the tests used in the present study are not extremely sensitive regarding changes in coagulation and also do not evaluate fibrinolysis. Other ways of measuring coagulation are available such as the thromboelastogram that allows evaluation of the coagulation as well as the fibrinolysis. In 2008, Steffens et al. [19] evaluated the use modified ultrafiltration using the thromboelastogram in adults and also found no differences between the control group and the MUF group. This study, however, consists of only 19 patients in total, being nine patients in the control group and 10 in the MUF group; being that the findings can be related to the size of the sample.
MUF has several reports in literature regarding removal of inflammatory mediators that may contribute to the decrease in inflammatory response. Antunes et al. [20], in a prospective study with conventional ultrafiltration, showed removal and decrease of inflammatory factors in patients submitted to coronary artery bypass graft surgery, but with no difference concerning the clinical resulting the studied groups.
Although less need for transfusion in the MUF group and less postoperative bleeding, we observed no clinical differences between both groups. The hospitalization and intensive care unit stay time was the same in both groups. These observations are in compliance with previous reports that evaluated conventional ultrafiltration or the association of conventional and modified ultrafiltration in the same patient [12,21,22].
Our study has limitations regarding the non-measurement of inflammatory mediators. The measurements of respiratory mechanics were only performed in the intraoperative period due to the difficulties of measurement in the intensive care unit with the extubated patients. Furthermore, the respiratory mechanics data are not comparable between the intraoperative period and the intensive care unit period, for the patients are no longer under mechanical ventilation. Our observation was limited to the hospitalization period without long-term follow-up; however, during this period MUF had proven to be safe for application.
Summing up; the modified ultrafiltration technique can be used frequently in adult patients as it is already been used in pediatric patients with safety. The most evident benefits are related to less need for blood transfusion and less postoperative bleeding, however, both groups presented similar clinical evolution. Modified ultrafiltration perhaps plays a more important role in manipulating fluids in the intraoperative of patients with poor ventricular function. Further investigation is necessary in order to define the MUF function as a mean of improving postoperative recovery.
REFERENCES
1. Liebold A, Keyl C, Birnbaum DE. The heart produces but the lungs consume proinflammatory cytokines following cardiopulmonary bypass. Eur J Cardiothorac Surg. 1999;15(3):340-5. [MedLine]
2. Chew MS, Brandslund I, Brix-Christensen V, Ravn HB, Hjortdal VE, Pedersen J, et al. Tissue injury and the inflammatory response to pediatric cardiac surgery with cardiopulmonary bypass: a descriptive study. Anesthesiology. 2001;94(5):745-53; discussion 5A.
3. Radaelli A, Loardi C, Cazzaniga M, Balestri G, DeCarlini C, Cerrito MG, et al. Inflammatory activation during coronary artery surgery and its dose-dependent modulation by statin/ACE-inhibitor combination. Arterioscler Thromb Vasc Biol. 2007;27(12):2750-5. [MedLine]
4. Perrotta S, Lentini S. Ministernotomy approach for surgery of the aortic root and ascending aorta. Interact Cardiovasc Thorac Surg. 2009;9(5):849-58. [MedLine]
5. Allen M, Sundararajan S, Pathan N, Burmester M, Macrae D. Anti-inflammatory modalities: their current use in pediatric cardiac surgery in the United Kingdom and Ireland. Pediatr Crit Care Med. 2009;10(3):341-5. [MedLine]
6. McEvoy MD, Sabbagh MJ, Taylor AG, Zavadzkas JA, Koval CN, Stroud RE, et al. Aprotinin modifies left ventricular contractility and cytokine release after ischemia-reperfusion in a dose-dependent manner in a murine model. Anesth Analg. 2009;108(2):399-406. [MedLine]
7. Naik SK, Knight A, Elliott MJ. A successful modification of ultrafiltration for cardiopulmonary bypass in children. Perfusion. 1991;6(1):41-50. [MedLine]
8. Brancaccio G, Villa E, Girolami E, Michielon G, Feltri C, Mazzera E, et al. Inflammatory cytokines in pediatric cardiac surgery and variable effect of the hemofiltration process. Perfusion. 2005;20(5):263-8. [MedLine]
9. Boodhwani M, Williams K, Babaev A, Gill G, Saleem N, Rubens FD. Ultrafiltration reduces blood transfusions following cardiac surgery: a meta-analysis. Eur J Cardiothorac Surg. 2006;30(6):892-7. [MedLine]
10. Maluf MA, Mangia C, Bertuccez J, Silva C, Catani R, Carvalho W, et al.. Estudo comparativo da ultrafiltração convencional e associação de ultrafiltração convencional e modificada na correção de cardiopatias congênitas com alto risco cirúrgico. Rev Bras Cir Cardiovasc. 1999;14(3):221-36. View article
11. Castro RP, Croti UA, Machado MN, Murillo HG, Rincon OYP, Policarpo SR, et al. Ultrafiltração convencional com modificação técnica no tratamento cirúrgico dos defeitos cardíacos congênitos. Rev Bras Cir Cardiovasc. 2006;21(1):42-9. View article
12. Luciani GB, Menon T, Vecchi B, Auriemma S, Mazzucco A. Modified ultrafiltration reduces morbidity after adult cardiac operations: a prospective, randomized clinical trial. Circulation. 2001;104(12 Suppl 1):I253-9. [MedLine]
13. Ornato JP, Peberdy MA. Cardiopulmonary resuscitation. Totowa:Humana Press;2005.
14. Westaby S. Organ dysfunction after cardiopulmonary bypass. A systemic inflammatory reaction initiated by the extracorporeal circuit. Intensive Care Med. 1987;13(2):89-95. [MedLine]
15. Smetkin AA, Kirov MY, Kuzkov VV, Lenkin AI, Eremeev AV, Slastilin VY, et al. Single transpulmonary thermodilution and continuous monitoring of central venous oxygen saturation during off-pump coronary surgery. Acta Anaesthesiol Scand. 2009;53(4):505-14. [MedLine]
16. Mahmoud AB, Burhani MS, Hannef AA, Jamjoom AA, Al-Githmi IS, Baslaim GM. Effect of modified ultrafiltration on pulmonary function after cardiopulmonary bypass. Chest. 2005;128(5):3447-53. [MedLine]
17. Song LO, Yinglong LI, Jinping LI. Effects of zero-balanced ultrafiltration on procalcitonin and respiratory function after cardiopulmonary bypass. Perfusion. 2007;22(5):339-43. [MedLine]
18. Pérez-Vela JL, Ruiz-Alonso E, Guillén-Ramírez F, García-Maellas MT, Renes-Carreño E, Cerro-García M, et al. ICU outcomes in adult cardiac surgery patients in relation to ultrafiltration type. Perfusion. 2008;23(2):79-87. [MedLine]
19. Steffens TG, Kohmoto T, Edwards N, Wolman RL, Holt DW. Effects of modified ultrafiltration on coagulation as measured by the thromboelastograph. J Extra Corpor Technol. 2008;40(4):229-33. [MedLine]
20. Antunes N, Dragosavc D, Petrucci Junior O, Oliveira PPM, Kosour C, Blotta MHSL, et al. Ultrafiltração para remover mediadores inflamatórios durante circulação extracorpórea na revascularização do miocárdio. Rev Bras Cir Cardiovasc. 2008;23(2):175-82. [MedLine] View article
21. Grunenfelder J, Zund G, Schoeberlein A, Maly FE, Schurr U, Guntli S, et al. Modified ultrafiltration lowers adhesion molecule and cytokine levels after cardiopulmonary bypass without clinical relevance in adults. Eur J Cardiothorac Surg. 2000;17(1):77-83. [MedLine]
Fundação de Amparo a Pesquisa de São Paulo - FAPESP
Article receive on Friday, October 30, 2009


 All scientific articles published at www.rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbccv.org.br are licensed under a Creative Commons license