Giovani José Dal Poggetto MolinariI; Andreia Marques de Oliveira DalbemI; Fábio Hüsemann MenezesII; Ana Terezinha GuillaumonIII
DOI: 10.5935/1678-9741.20140014
ABSTRACT
INTRODUCTION: Endovascular aneurysm repair requires the precise deployment of the graft. In order to achieve accurate positioning, the anatomical and morphological characteristics of the aorta and its branches is mandatory. Software that perform three dimensional reformatting of multislice tomographic images, allow for the study of the whole aorto-iliac axis and the perpendicular visualization of the origin of the renal arteries. The correct length of the proximal neck can be evaluated and adequate graft fixation and sealing may be foreseen. A technique is presented, using an software, for the orthogonal correction of the position of the renal arteries in relation to the proximal neck, which may guide the radioscopic orientation intraoperatively.
METHODS: Within a multiplanar tomographic image reconstruction, virtual triangulation allows for the three dimensional orthogonal correction of the renal arteries' ostia position. The predetermined best angulations for visualization are annotated and used for the positioning of the surgical C-arm.
RESULTS/DISCUSSION: Some authors discuss that the anatomic position of the renal vessels seen on the tomographic scan can change during the surgical procedure. It is known that the renal arterys' angular positioning does not alter, even after insertion of stiff guidewires, introducers, and the endograft itself. Therefore, it is possible, using concepts of spacial geometry and orthogonal correction, to predict the ideal bidimensional intraoperative positioning of the radioscopy device in order to reproduce the optimized renal artery ostial projection, ensuring the best accuracy during endograft deployment.
CONCLUSION: As closer to the tomographic reproduction was the radioscopic correction, more careful is the visualization of the ostium of the renal artery, better is the exploitation of the lap for fixing and sealing and the endoprosthesis deployment is more accurate.
RESUMO
INTRODUÇÃO: Para o preparo pré-operatório endovascular dos aneurismas infrarrenais é necessária a mensuração acurada de suas características anatômicas e morfológicas, alcançada com o uso de softwares avançados em manipulação de imagens de tomografias multicanais. Este processo permite também o estudo acurado das relações anatômicas das demais artérias do eixo aorto-ilíaco. Uma visualização perpendicular à origem da artéria renal mais baixa possibilita o uso de toda a extensão do colo para fixação da endoprótese e selamento proximal, o que pode ser previsto durante o estudo da tomografia, impedindo um posicionamento subótimo e a sobreposição das estruturas vasculares no intraoperatório. Expõem-se aqui os resultados iniciais de um projeto piloto, envolvendo manipulação de imagens tomográficas, na correção ortogonal da artéria renal aplicada à orientação radioscópica no intraoperatório.
MÉTODOS: Por meio de reconstrução multiplanar de imagens tomográficas em software obtém-se um corte axial em ângulo reto. Conceitos geométricos de triangulação virtual promovem a correção ortogonal em três dimensões da visualização ostial da artéria renal, que pode ser reproduzida intraoperatoriamente, através do reposicionamento do arco cirúrgico.
RESULTADOS/DISCUSSÃO: Embora alguns autores argumentem que a anatomia do vaso observada na tomografia possa mudar durante o intraoperatório, sabe-se que o posicionamento angular das artérias renais não se modifica, mesmo após a inserção dos fios guia rígidos, introdutores e da própria endoprótese. Assim, acreditamos ser possível, por meio de conceitos de geometria espacial e correção ortogonal (por meio da manipulação das imagens em software), predizer o posicionamento ideal do aparelho de radioscopia de maneira a reproduzir o mesmo ângulo de projeção ostial da artéria renal em imagem bidimensional intraoperatória (angiografia), assegurando maior precisão na liberação da endoprótese.
CONCLUSÃO: Quanto mais próxima da reprodução tomográfica for essa correção radioscópica, mais cuidadosa é a visualização do óstio da artéria renal, melhor é o aproveitamento do colo para a fixação e selamento e mais precisa é a liberação da endoprótese.
3D: Three Dimensions
AAA: Abdominal aortic aneurysm
DICOM: Digital Imaging and Communications in Medicine
h: Height
MIP: Maximum intensity projection
MPR: Multiplanar reconstruction
r: Radius
TC: Computed Tomography
INTRODUCTION
It is known that for the preoperative preparation of endovascular infrarenal abdominal aortic aneurysms (AAA) accurate measurement of morphological and anatomical characteristics of the aneurysm is required, such as diameters, lengths and angles, essential strategy for their exclusion, the final result endovascular procedure [1].
With the enhancement of information technology, the study of helical biplane CT scans associated with complementary marked catheter aortography was replaced by the use of computed tomography (CT) multichannel (multislice), with cuts in smaller thicknesses and with greater detail that, when associated with three dimensions (3D) reconstruction software, allow the scanned virtual reproduction of the patient and his anatomy [2].
CT and angiography (angioTC) have an essential role in preinterventional planning and control of the procedure and is considered the test of choice in assessing the candidate patient to envodascular treatment and for his monitoring in search of complications [3].
These reconstructions allow rapid assessment of the extent of the aneurysm, visceral involvement, presence of angulation, tortuosity and access difficult. An accurate analysis of the axial, coronal and sagittal sections enables the planning of the type of stent to be used. This is achieved with the use of reconstruction methods available in software such as multiplanar reconstruction (MPR and MPR - Curved), maximum intensity projection (MIP) and 3D image reconstruction volume.
At this stage, performed in the preoperative period, we obtain the necessary information for surgical planning. Thus, it is possible the acquisition of final images that offer not only better accuracy of measurements and morphological features of the aneurysm as well as the study of their anatomical relationship with the other arteries of the aortoiliac axis [1].
An important aspect of planning is determining the best intraoperative placement of fluoroscopy, with a perfectly perpendicular view to the origin of the lowest renal artery visualization. A suboptimal positioning can cause overlapping of vascular structures, preventing the use of the entire length of the colon to the fixation of the stent graft and proximal sealing [4].
The initial results of a pilot project are set herein, performed by examining the feasibility of manipulation of CT images in software, the visualization and determination of radioscopic angulation of the aneurysm neck, through the use of a new technique. It is believed that this technique is quite simple, of immediate practical significance and can be easily incorporated into routine planning of endovascular treatment with stents. So far, we have collected a series of cases of about 14 studies with encouraging results. For purposes of illustration of the technique used, the steps developed in one case in our series are following described.
METHODS
Multichannel CT scans of patients undergoing endovascular repair of infrarenal AAA at the Center for Highly Complex Endovascular Surgery, State University of Campinas, from August to December 2013 were assessed.
We used three-dimensional multiplanar reconstruction through DICOM - Digital Imaging and Communications in Medicine image manipulation software (OsiriX MD), in analysis of aneurysms in serial CT images with fine cuts of 1 to 3mm, through intravenous iodinated contrast in the arterial phase.
We chose the lowest renal artery as a reference for the treatment of images because the proximal colon constituted its thread until the start of the AAA [5]. The aim was to achieve a perfectly perpendicular image to its source, or that is, its ostial projection, to correct anteroposterior angulation inherent to its morphology and any rotational effects caused by tortuosity of AAA. For this, a linear axis of the aorta (at the level of the emergence of the lowest renal artery) cut was achieved in axial image, provided by the right-angle correction of the sagittal and coronal MPR projections (Figure 1).

Upon analysis of the axial image, we then proceeded to construct a circumscribed equilateral triangle. Was traced a centerline axis of the aorta and parallel to the tangent of the arterial wall in the renal ostium where a first mark made in the anterior wall of the aorta was performed (Figs. 2A and 2B). This vertex is assumed to be the apex of the pyramid at the beginning of the construction of the triangle. Therefore, we reproduced two additional marks guided by the height of the triangle placed subsequently in order to form an equilateral triangle (Figure 2C). To calculate the markup, we used the concepts of geometric construction, where the height (h) of an equilateral triangle in a circle corresponds to ¾ diameter, or 1 ½ time the radius of the circle [6] (r) (Figure 2D).
.jpg)
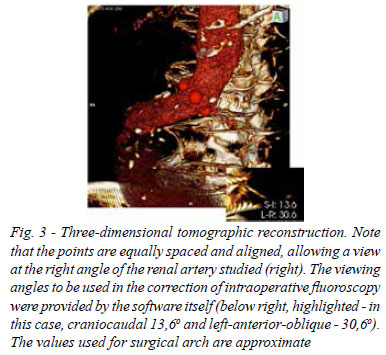
Starting with the geometric concept that three points are always coplanar, we proceeded to the three-dimensional reconstruction of CT. By means of rotational manipulation of the image if the three aligned points along a single axis, equidistant (Figure 3). The projection angles of the image display were provided automatically by the software (highlighted).
The images and angles achieved during the 3D reconstruction software were reproduced during surgery - with correction of angular positioning of the fluoroscopy unit – and were considered equivalent (Figures 4A , B and C).
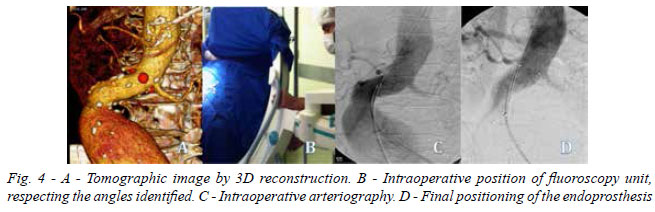
We can also mention that for prostheses that have above two radiopaque markers at the same level at the proximal portion, it could be observed after the release of the stent, a placement in a straight position to these markings [ 4 ] which reinforces the idea of perpendicular view of the cervix (Figure 4D).
DISCUSSION
Early in the last decade, the study of helical CT combined with complementary biplanar aortography with marked catheters was recommended to all candidates for endovascular repair of AAA, by presenting themselves as complementary examinations values: while the first provided very accurate information about the diameters, the last allowed an accurate assessment of the length [7].
Due to the high technological development of the CT - since the introduction of helical acquisition to multichannel detectors equipment with efficient systems of transmission, processing and storage of data - it was possible to reduce the time of image acquisition and the development of more sensitive and accurate algorithms, with better performance and spatial resolution [2] reconstruction.
Currently, through angioTC the morphometry is performed, based on the assessment of the configuration, lengths and diameters of the aorta and iliac arteries and related to the lesion of interest as to the technique of performing the endovascular procedure. It allows even assess relevant anatomical variations when choosing the stent and the related surgical technique [2].
However, the intraoperative assessment of the release of the stent is usually guided by angiography, which provides two dimensional image. Therefore, it is known that the proximal neck of AAA and/or too angulated iliac arteries may hinder accurate visualization of the ostium of the renal artery.
The ideal positioning of the fluoroscopy unit during the surgical procedure may be different than expected during the preoperative study, in that the aneurysm possibly shorten or lengthen higher than expected [4]. Thus, some authors argue that the anatomy of the vessel can change due to the insertion of rigid guidewires, introducers and the delivery system itself. They believe that the image of the preoperative CT may be different from intraoperative angiography [6].
Van Keulen et. al. [4] discuss about the necessity of determining the intraoperative disposition of surgical arch arguing that a suboptimal positioning would lead the surgeon to underestimate the total length of the aneurysm neck and not using in its entirety for release and fixation of the endoprosthesis. This interpretation could be caused by an apparent overlap of vascular structures in the conventional biplane angiographic image. They recommend that the ideal angulation and positioning are determined taking into account the anteroposterior angulation of the neck and the clockwise orientation of the renal arteries. They also report that although the angulation of the neck of the aneurysm can be changed, the angular position of the renal arteries is not changed even under the influence of the inserted guide wire or the stent itself [4,8].
Our aim was to simplify this calculation, with simultaneous attainment of oblique and craniocaudais angles using concepts of three-dimensional geometry and spatial triangulation with the aid of software. That said, although the results are result from a pilot project underway, these proved to be very encouraging.
Therefore, we believe that it is possible, by means of concepts of geometric correction and through manipulation of DICOM images in software, to trace the same angle of ostial projection of the renal artery on intraoperative two-dimensional image (angiography).
When playing a tomographic cross section at right angles (or that is, perpendicular to the axis of the aorta), with rotation and orthogonal exposure of the renal artery, it is possible to predict the need for intraoperative correction of the fluoroscopy projection in obtaining two-dimensional angiographic image.
Utilizing the application of concepts of spatial geometry to achieve the best angle of ostial exposure of the renal artery systematically, it may reduce the variations between study observers and allows the reproducibility of the technique, reducing errors of interpersonal interpretation.
The closer this radioscopic correction of the tomographic reproduction, the more careful the visualization of the ostium of the renal artery, and the better the exploitation of the neck for fastening and sealing and the more accurate the endoprosthesis deployment.
REFERENCES
1. Oderich GS, Malgor RD. Aneurisma da Aorta toracoabdominal. In: Lobato AC (org). Cirurgia Endovascular. 2nd ed. São Paulo: Instituto de Cirurgia Vascular e Endovascular de São Paulo; 2010. p.695-742.
2. Pitoulias GA, Donas KP, Schulte S, Aslanidou EA, Papadimitriou DK. Two-dimensional versus three-dimensional CT angiography in analysis of anatomical suitability for stentgraft repair of abdominal aortic aneurysms. Acta Radiol. 2011;52(3):317-23. [MedLine]
3. Kuroki IR, Magalhães FV, Rizzi P, Coreixas IMH. Angiotomografia. In: Brito CJ. Cirurgia Vascular: cirurgia endovascular, angiologia. 3ª ed. Rio de Janeiro: Revinter; 2014. p.437-96.
4. van Keulen JW, Moll FL, van Herwaarden JA. Tips and techniques for optimal stent graft placement in angulated aneurysm necks. J Vasc Surg. 2010;52(4):1081-6. [MedLine]
5. Lobato AC. Aneurisma da Aorta Infrarrenal. In: Lobato AC (org). Cirurgia Endovascular. 2nd ed. São Paulo: Instituto de Cirurgia Vascular e Endovascular de São Paulo; 2010. p.743-96.
6. Rigonatto M. Triângulo equilátero inscrito numa circunferência. [cited 2013 Mai 22]. Available from: http://www.mundoeducacao.com/matematica/triangulo-equilatero-inscrito-numa-circunferencia.htm
7. Espinosa G, Marchiori E. Araújo AP, Caramalho MF, Barzola P. Abdominal aorta orphometric study for endovascular treatment of aortic aneurysms: comparison between spiral CT and angiography. Rev Bras Cir Cardiovasc. 2002;17(4):323-30.
8. van Keulen JW, Moll FL, Tolenaar JL, Verhagen HJM, van Herwaarden JA. Validation of a new standardized method to measure proximal aneurysm neck angulation. J Vasc Surg. 2010;51(4):821-8. [MedLine]
No financial support.
Roles & authors' responsibilities
GJDPM: Lead author, creator of the technique described. Principal investigator for the manipulation of images used, writing of the Pilot Project and Research Project and bibliographic survey.
AMOD: Coauthor. Collaborative development and application of this technique, assistant researcher in the development of the Research Project.
FHM: Coauthor. Reviewer of writing Technical Note, correction and preparation of the Abstract. Reviewer of references.
ATG: Coauthor. Guidance. Final reviewer of Technical Note, Pilot Project and Research Project.
Article receive on Friday, August 30, 2013
 All scientific articles published at www.rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbccv.org.br are licensed under a Creative Commons license