To evaluate the pain in patients submitted to heart surgery using sternotomy, verifying the location and intensity of pain during the hospitalization period. A second aim was to evaluate its influence on the pulmonary function and its correlation with the characteristics of the individual and the surgical procedure.
The series was composed of 30 individuals with the preoperative pulmonary function assessed by spirometry and incentive spirometry. Patients were followed in the postoperative period using a protocol with information on the surgery and the pulmonary function and a protocol for pain evaluation (visual analogue scale and body picture). Descriptivestatistics, Mann-Whitney test and Spearman correlation were used for statistical analysis.
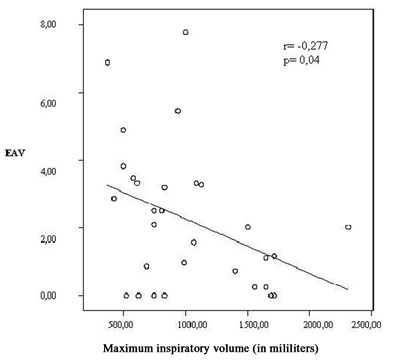
Coronary artery bypass surgery was the most frequent surgery. The pain intensity in the postoperative period was moderate, initially located near to the sternotomy and persisted until the 5th postoperative day. The maximum inspiratory volume had a significant relationship with pain (r= -0.277; p< 0.05). No significant correlation was observed between pain and others parameters.
Significant damage to the pulmonary function is observed which does not completely recover until the 5th postoperative day. Despite these results, pain is not significantly associated to the characteristics of the individual or the surgical procedure.
Avaliar a dor em pacientes submetidos à cirurgia cardíaca por esternotomia, verificando a localização e a intensidade da dor durante o período de internação. Também sua influência na função pulmonar e sua correlação com as características do indivíduo e do procedimento cirúrgico.
A amostra foi composta de 30 indivíduos, nos quais foi avaliada a função pulmonar pré-operatória por espirometria e inspirometria de incentivo. Acompanharam-se os pacientes no pós-operatório, por meio de protocolo com informações da cirurgia, função pulmonar e um protocolo de avaliação álgica (escala análoga visual e desenho do corpo humano). Utilizou-se estatística descritiva, o teste de Mann-Whitney e a correlação Spearman.
A revascularização do miocárdio foi a cirurgia mais freqüente. A intensidade da dor no período de pós-operatório foi moderada e localizava-se inicialmente na esternotomia, persistindo até o 5º pós-operatório. O volume inspiratório máximo teve relação significativa com a dor (r= -0,277; p< 0,05). Não se observou correlação significativa da dor com outras variáveis.
Observou-se prejuízo significativo da função pulmonar, não se restabelecendo completamente até o 5º dia de pós-operatório. Apesar dos achados, a dor não se relacionou significativamente com as características dos indivíduos e do procedimento cirúrgico.
INTRODUCTION
Pain is a common sensation after heart surgery. Mueller et al. [1] reported that 51% of patients still suffer from pain in the region of the sternotomy on the 7th day after surgery. Walther et al. [2] also reported that a relatively high number of patients complain of pain during the same period. Other works on the subject show that the incidence of moderate pain affects 43% and severe pain 34% of patients depending on the conduct of the service [3,4].
In spite of these findings, between 50% and 75% of patients do not receive adequate analgesic support, leading to an increased risk of sympathic activity and ischemic events [3,5]. Additionally, episodes of nausea and vomiting, restriction of movements and a resulting increase in the chance of thromboembolism are reported [5], causing prolonged hospitalization times with consequently higher costs that exceed 28,000 Euros per patient in some countries [6,7].
Pain originating from routine postoperative procedures associated with great nociceptive stimulation of the sternotomy is a significant cause of morbidity and mortality in this period [5,8], as it influences the capacity to cough, breathe and adequately move and may result in atelectasis (occurring in up to 90% of patients in the lower left lobe) and pneumonia (29%) [9,10].
Longitudinal median sternotomy was first performed in 1958 and is the most commonly used incision in heart surgery [11] as it is the best procedure to expose the region however, it can significantly alter the pulmonary function due to consequent instability of the upper thorax [12,13]. The use of the left internal thoracic artery (LITA) is also associated to changes in pulmonary function as this graft involves additional surgical trauma and is more painful for the patient implicating a specific clinic condition [1,12].
In spite of all the technical advances in recent years, pain in the postoperative period still seems to be underestimated. Many patients do not request analgesics, even presenting with much pain and others receive only 47% of the effective dose of analgesic according to data presented by the study of Watt-Watson et al. [3]. Through education, the use of analgesics might become more conscientious and in some cases, its restricted use by the patient may become more efficient. An understanding of the characteristics of pain in the postoperative period and its influence are necessary to develop strategies to control it better.
Thus, the objective of this study is to evaluate pain in adult patients submitted to heart surgery using sternotomy, verifying the location and the intensity of pain during the period of hospitalization. Also its influence on pulmonary function and its correlation with the characteristics of the individual and the surgical process were assessed.
METHOD
This is a cross-sectional, quantitative, longitudinal and prospective study with a non-probabilistic sample carried out between March and December 2005 in Irmandade Santa Casa de Misericórdia de Porto Alegre (ISCMPA). This work was approved by the Ethics Committees of the institutions involved in Porto Alegre: Centro Universitário Metodista and ISCMPA.
Initially 120 patients were selected for the study. Of these 79 were excluded as they did not fulfill the inclusion criteria: 51% of the patients had already been submitted to one or more heart surgeries, 17% had already been submitted to other thoracic surgeries, 9% of the individuals did not undergo sternotomies, 9% of the patients refused to participate in the study, 6% presented with Class III unstable angina (Braunwald classification), 6% were operated on under urgency or emergency conditions (impossible to collect preoperative data) and 2% of the individuals presented with mediastinal cancer.
The patients were included after an interview to explain the nature of the work and after signing written consent forms. Forty-one patients participated in the study however 11 did not complete all of the stages and were considered lost to the study (for retracting consent, surgeries postponed to dates after completion of the study or cancelled and death).
The analyzed sample composed 30 individuals with a mean age of 53.9 ± 13.93 years including both genders who were electively submitted to coronary artery bypass graft (CABG) or valve surgery by sternotomy (both on-pump and off-pump) and who were extubated according to the standard routine of the service. No patient presented with acute pulmonary disease at the moment of the study.
A preoperative evaluation was made which consisted of data collection including the patients name and detailed information about risk factors and associated diseases. Additionally the pulmonary function was evaluated by means of spirometry and incentive inspirometry (to obtain an estimation of the maximum inspiratory capacity).
Pulmonary function (spirometer - Micro Medical Limited ®) supplied the forced vital capacity (FVC), the forced expiratory volume at one second (FEV1), coefficient of the forced expiratory volume at one second (FEV1/FVC%) and peak expiratory flow (PEF). With this, patients were requested to make a forced expiration from total lung capacity. To obtain the maximum inspired volume (maxIV), incentive inspirometry was performed (Voldyne ®) after 15 minutes resting. The patient was asked to breathe slowly but deeply to expand the abdomen from functional residual capacity. Incentive inspirometry was selected due to its low cost and easy reproducibility. For both tests, three maneuvers at one-minute intervals were performed. The patients were evaluated seated in bed with the head of the bed at an angle between 45º and 90º. The seated position was avoided when the individual was excessively heavy (body mass index equal to or greater than 35 kg/m2). The head of bed was reclined at 30º in these cases. Spirometry followed the criteria established by the guidelines for pulmonary function tests [14]. The highest reading was adopted, as long as it presented with a difference of less than 10% compared to the second highest reading.
The patients were accompanied on the first, second, third and fifth postoperative days. The follow-up protocol consisted in information on the characteristics of the surgical procedure and data on the pulmonary function. When the patient complained of pain, a specific protocol was utilized for its evaluation before the pulmonary function tests. This protocol comprised drawings of the front and back views of a human body divided into 37 anatomical regions. The patient was requested to mark the region with most pain. Additionally, a visual analogous subjective scale from 0 to 10 was applied for that region with 0 representing no pain and 10 the most intense pain possible (pain assessment protocol utilized by Mueller et al. [1]).
All patients were transferred from the surgical room with nº 36 thoracic drains (Braile®mark) at variable locations, but only five patients were still utilizing the drain at the start of data collection. Thus, it was difficult to statistically evaluate its influence on pain.
In the immediate postoperative period, the analgesia utilized by the service consisted in morphine (from 2 to 10 mg diluted in 9 mL of distilled water increased by 1 mL of morphine every 4 hours). Infusion was continuous from 2 to 5 mg per hour when necessary. After this period, 750 mg paracetamol (first line) when necessary or paracetamol associated to codeine (at 4 hour intervals) was utilized. Dipyrone (2 mL) was used when necessary diluted in 8 mL of distilled water.
Analysis of the data was attained by descriptive statistics using means and standard deviation. Continuous variables without normal distributions were presented as medians and interquartile 25-75 percentiles. The Mann-Whitney non-parametric test was utilized for variables without normal distribution (characteristics of individuals) and Spearman coefficient for the analysis of intensity of associations between the variables (pulmonary function and characteristics of the surgical procedure). A significance level of 5% (p<0.05) was employed. Data were analyzed using the SPSS program versions 12.0 and 13.0.
RESULTS
Thirty patients participated of the study with 73.3% being men. The mean ejection fraction was 61 ± 13.9%. Systemic arterial hypertension (SAH) was most prevalent (76%) in patients with associated diseases (followed by dyslipidemia at 28%, diabetes mellitus and previous acute myocardial infarction, both with frequencies of 20%). Chronic obstructive pulmonary disease (COPD) was also prevalent (16.7%). Thirty per cent of patients were smokers with an average of 23.7 ± 13.93 years of smoking and an average consumption of around of 28.5 cigarettes per day. None of the patients had previously been submitted to upper abdominal surgery and 36.7% performed preoperative physiotherapy. The characteristics of the patients and the main risk factors for postoperative complications are presented in Table 1.

The surgical procedures performed were coronary artery bypass grafting (CABG), valve replacement (49%) and partial valve resection (1%). Forty per cent of the CABG procedures involved the LITA, 10% involved the saphenous vein and 30% of the replaced valves were metallic. Most of the patients (76.7%) used CPB. The characteristics of the surgical procedures are also showed in Table 1.
The mean values of FEV1 and of FVC in the preoperative period were from l.9 ± 0.75 and 2.8 ± 1.05 liters, respectively. On the 1st postoperative day, the values decreased significantly to 0.66 ± 0.25 and 1.0 ± 0.36 liters (p<0.001 in relation to the preoperative period). The FEV1 increased significantly from the 2nd postoperative day (0.83 ± 0.34 liters, p<0.001 and on the 3rd postoperative day 1.09 ± 0.4 liters; p<0.001) until the 5th postoperative day (1.23 ± 0.58 liters; p= 0.047). The FVC also increased significantly every day from 2nd postoperative day (1.17 ± 0.46 liters, on the 2nd postoperative day and 1.44 ± 0.48 liters on the 3rd postoperative day, both p=0.0011) until the 5th postoperative day (1.71 ± 0.62 liters, p=0.008). The statistical differences for these variables are in relation to the 1st postoperative day.
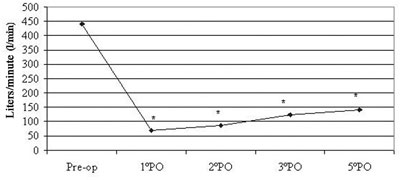
The mean value of the PEF in the preoperative period was 163 ± 71.49 liters/minute with a significative drop to 69.38 ± 25.21 liters/minute on the 1st postoperative day (p<0.001). The values increased significantly every day compared with the 1st postoperative day. On the 2nd postoperative day, the PEF was 86.06 ± 35.63 liters/minute and on the 3rd postoperative day it was 122.89 ± 63.06 liters/minute (both giving p=0.001). On the 5th postoperative day, this value reached 141.07 ± 76.71 liters/minute (p=0.026) - Figure 1. In the preoperative period, the mean MaxIV was 2266.6 ± 900.03 milliliters, which reduced significantly to 646.15 ± 284.57 milliliters on the 1st postoperative day (p<0.001). Similar to the other pulmonary function parameters, there were a significant increases on the 2nd and 3rd postoperative days (933.92 ± 496.47 milliliters and 1265.38 ± 713.69 - both p<0.001). On the 5th postoperative day it was 1425.96 ± 732.27 milliliters (p= 0.089 compared to the 1st postoperative day).
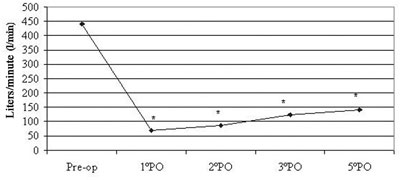
Fig. 1 - Mean values of peak expiratory flow. * p<0.05 between the pre and the 1st postoperative day, between the 1st and the 2nd postoperative day, between the 2nd and the 3rd postoperative day and the 3rd and 5th postoperative days
Only five patients did not present pain during all the postoperative period; on the 1st day, 17 (56.6%) patients suffered from pain, on the 2nd day 18 (60%) individuals had pain and on the 3rd day only nine (30%). On the 5th day after surgery, 11 (36.6%) patients still felt pain. Moderate pain (6.17 ± 3.04) was reported on the 1st postoperative day and this significantly decreased (p=0.003) on the 2nd postoperative day (3.95 ± 2.23, mild pain), but increased again on the 3rd postoperative day (4.67 ± 3.57, p=0.859) and remained moderate until the 5th postoperative day (4.7 ± 3.60, p= 0.547). The most reported site of the pain was the sternal region, except on the 5th postoperative day, with the upper region of the left leg (corresponding to the region next to the quadriceps) being reported as the most painful region (n=3/11) even by patients who utilized LITA grafts.
When pain was correlated to the characteristics of the individuals, there was no significance between the intensity of pain and gender (p=0.87), age (p=0.387) or BMI. Also when the pain was correlated to the characteristics of the surgery, no significances were observed with any of the variables, for example, between the intensity of pain and the time of intubation (p=0.248). The type of surgery was not associated to the intensity of pain (p=0.970), nor was the surgical time (p=0.812) or CPB time (0.07).
The time of analgesia was not statistically different on any of the postoperative days (p=0.9 for the 1st and 2nd postoperative days; p=0.490 for the 3rd postoperative day and p=0.760 for the 5th postoperative day). The connection between the use of analgesics and intensity of pain was significant on the 1st postoperative day (p=0.013), which can be explained by the high average pain on this day (6.17 ± 3.04).
A correlation close to significant, though weak, was found between the intensity of pain and PEF (r = -0.360; p = 0.051); and, although significant, the correlation between pain intensity and MaxIV was also weak (r = 0.277; p = 0.04) - Figure 2.
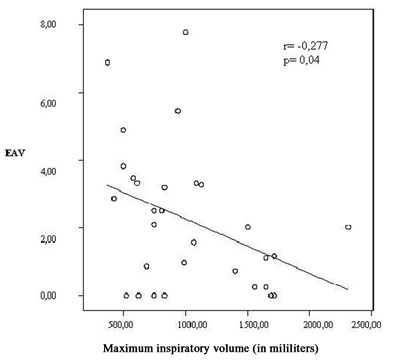
Fig. 2 - Relationship between pain intensity and maximum inspiratory volume, r = -0.277; p= 0.04. VAS - visual analogous scale
In the current study we did not observe significant associations between individual characteristics (age, gender and BMI, for example) and surgical procedure, as has been reported by some authors, maybe because of the small sample size. Mueller et al. [1] reported that under 60-year-old patients suffered more pain with a mean of 4.3 ± 2.2 (3.6 ± 2.4 for over 60-year-old patients). The causes are not precise, but it is suggested that perhaps the difficulty of communication of elderly people may be the reason of these findings. On the other hand, in another work by the same authors [15], elderly patients had higher mean intensities of pain, but, in this study the use of LITA grafts was prevalent in patients of this age range. Likewise, the reasons for the difference between genders and pain are contradictory. Individuals who presented with BMIs of more than 30 kg/m2 also suffered more pain, possibly due to difficulty in providing sufficient analgesics [1]. Statistical assessment of this variable was not possible in our work, as only three patients had BMIs of greater than 30 kg/m2. In the studies of Mueller et al. [1] and Watt-Watson et al. [3], women presented with more pain. In this latter study, the fact was explained by the lower frequency of requests for analgesics by female patients in the postoperative period. As only eight women participated in our study the assessment of this variable is difficult.
Confirming the findings of Mueller et al. [1, 15], the level of pain mentioned in this current study was moderate (except on the 2nd postoperative day) and was sited in the region of the sternotomy until the 3rd postoperative day, passing to the leg associated to the saphenectomy (in the case of the Mueller study, the pain starts to have osteoarticular characteristics). According to these two works, the greatest pain occurred on the 2nd postoperative day, however, in our study, the 1st postoperative day presented more pain. This variation of the site and intensity of pain may occur because the initial nociceptive stimulations that decreased with time (sternal instability and use of drains, for example) and as the patient becomes more active in bed, he feels other aspects related to the surgery such as the lack of moving, effect of muscle spasms related to the procedure and rib fractures [1, 3, 15]. We confirmed, in our research, that more patients suffered from pain on the 1st postoperative day than on the 5th postoperative day (17 and 11, respectively) and this emphasizes the importance of a more controlled initial analgesia.
Mueller et al. [1] in their study, similar to us, did not find any significant difference in the characteristics of pain among different types of surgery even when comparing deeper procedures, with more nociceptive stimuli such as valve surgeries, however they did not mention whether their patients underwent CABG utilizing LITA grafts. Nevertheless, the same author, in another work [15], compared patients who performed CABG using LITA and other grafts verifying that the mean pain of the patients who received LITA grafts was higher, maybe due to the additional surgical trauma that this graft causes. Possibly, in the current study, this relationship would be significant, with a larger sample size.
The significant impairment of pulmonary function in the postoperative period of heart surgery is a well known complication, but its causes are still being explored. Mueller et al. [15] affirm that the impact of LITA is moderate in the postoperative period, based on the greater surgical trauma that this graft causes (greater discomfort to the patient), but the authors did not perform pulmonary function tests. Çimen et al. [12] & Guizilini et al. [16] identify CPB as one of the causes due to the increase in airway resistance and a possible increase of diaphragmatic dysfunction, comparing the pulmonary function of patients who were submitted to on-pump and off-pump surgeries. Both showed that there is impairment after heart surgery, but the damage is greater in on-pump procedures. Thoracic drains also cause significant changes to the FEV1 and FVC as was reported by Guizilini et al. [17], with the intercostal drain being the worst when compared to mediastinal drains, due to the friction caused during respiration. Consequently, there is nerve irritation, causing more suffering to the patient. The incision itself is also considered by Walther et al. [2] and Lichtenberg et al. [13], who showed that a mini-incision causes less impairment to the pulmonary function than median sternotomy, thereby causing less pain, making early movement possible because of the sternal stability. But we can not affirm this in the current study, as it was not one of our objectives.
In the current work, a weak significant correlation between pain and MaxIV was shown confirming earlier studies on damage to the pulmonary function in the postoperative period of heart surgery. This finding confirms that changes in pulmonary function are also due to pain. The presence of thoracic drains, in particular intercostal, perforating the intercostal pleura and intercostal muscles [17] and limiting inspiration, is one cause. In our study, few patients were still using thoracic drains at the moment of data collection, and so, it is very difficult to suggest that drain use contributes to a significant reduction in MaxIV.
Additionally, the use of LITA grafts, although our study did not identify any association between these variables, may influence the inspiratory capacity. This happens because of the additional surgical trauma and reduction in blood to the intercostal musculature, reducing the ventilatory muscle force [15, 18]. Another possibility is diaphragmatic dysfunction caused by the surgery itself, that determines involvement of the phrenic nerve (maybe by cardioplegia) and diaphragmatic paresis [5,16]. However, this needs to be investigated further.
Heart surgery is a procedure that causes aggression to the organism. In spite of the influence of sternotomy on pain not being evaluated, this may be attributed to the extension of the incision [4,13] and friction of the sternum due to instability of the upper thorax [2, 16]. The low spirometric values together with and low but significant values of the maximum inspiratory capacity may also reflect the fear or indifference of patients to collaborate with the pulmonary function tests.
With adequate analgesic management, pain and consequently the postoperative pulmonary function can improve [5,15]. This is important, especially in the elderly, who already have a reduced pulmonary capacity (with higher risk of developing pulmonary complications). Additionally, with the advances in medicine there is an increase in the number of elderly patients undergoing surgical procedures.
In our study, we did not perform radiological assessments, which might show pulmonary complications that affect the pulmonary function. Moreover, the analgesic protocol utilized by the institution where the research was performed is different to in some works found on this subject, which employ epidural analgesia, thus comparisons among results are difficult. The pulmonary function tests represent a limitation, as mentioned before, as their results depend on specific maneuvers and on the desire of patients to perform them. The method to evaluate the maximum inspiratory capacity is no more specific but it is easy, reproducible and cheap.
Earlier works suggest that more prepared patients and those who collaborative better with the rehabilitation team can identify pain at an earlier stage [18]. As pain is a frequent symptom in postoperative heart surgery, professionals involved in rehabilitation of patients must also be educated in respect to this, aiming at identifying pain and its early management.
CONCLUSION
In this study, moderate pain was initially felt in the region of the sternotomy. But, pain was not correlated to the characteristics of individuals or to the surgical procedure, perhaps because of the sample size, as some variables have frequencies excessively small to calculate statistical significance. Even so, impairment of pulmonary function was verified, which was not stable on the 5th postoperative day. This change can best be observed with a significant association of pain with MaxIV. Additionally, pain was a complaint that persisted during the entire study period.
REFERENCES
1. Mueller XM, Tinguely F, Tevaearai HT, Revelly JP, Chiolero R, Segesser LK. Pain location, distribution, and intensity after cardiac surgery. Chest. 2000;118(2):391-6.
2. Walther T, Falk V, Metz S, Diegeler A, Battellini AR, Autschbach R, et al. Pain and quality of life after minimally invasive versus conventional cardiac surgery. Ann Thorac Surg. 1999;67(6):1643-7.
3. Watt-Watson J, Stevens B, Katz J, Costello J, Reid GJ, David T. Impact of preoperative education on pain outcomes after coronary artery bypass graft surgery. Pain. 2004;109(1-2):73-85.
4. Power I. Recent advances in postoperative pain therapy. Br J Anaesth. 2005;95(1):43-51.
5. Magnano D, Montalbano R, Lamarra M, Ferri F, Lorini L, Clarizia S. Ineffectiveness of local wound anesthesia to reduce postoperative pain after median sternotomy. J Card Surg. 2005;20(4):314-8.
6. Reimer-Kent J. From theory to practice: preventing pain after cardiac surgery. Am J Crit Care. 2003;12(2):136-43.
7. Pasquina P, Tramer MR, Walder B. Prophylactic respiratory physiotherapy after cardiac surgery: systematic review. BMJ. 2003;327(7428):1379-85.
8. Mueller XM, Tinguely F, Tevaearai HT, Ravussin P, Stumpe F, von Segesser LK. Impact of duration of chest tube drainage on pain after cardiac surgery. Eur J Cardiothorac Surg. 2000;18(5):570-4.
9. Abboud C. Infecção em pós-operatório de cirurgia cardíaca. Rev Soc Cardiol Estado São Paulo. 2001;5:915-21.
10. Johnson D, Kelm C, Thomson D, Burbridge B, Mayers I. The effect of physical therapy on respiratory complications following cardiac valve surgery. Chest. 1996;109(3):638-44.
11. Anger J, Farsky PS, Amato VL, Abboud CS, Almeida AF, Arnoni RT, et al.. A utilização de retalho composto de pele e tecido mamário na reparação da área cruenta resultante da deiscência de esternotomia em cirurgia cardíaca. Arq Bras Cardiol. 2004;83:43-5.
12. Çimen S, Özkul V, Ketenci B, Yurtseven N, Günay R, Ketenci B, et al. Daily comparison of respiratory functions between on-pump and off-pump patients undergoing CABG. Eur J Cardiothorac Surg. 2003;23(4):589-94.
13. Lichtenberg A, Hagl C, Harringer W, Klima U, Haverich A. Effects of minimal invasive coronary artery bypass on pulmonary function and postoperative pain. Ann Thorac Surg. 2000;70(2):461-5.
14. Pereira CAC, Jansen JM, Barreto SSM, Marinho J, Sulmonett N, Dias RM. Espirometria. In: Diretrizes para testes de função pulmonar. J Pneumol. 2002;28(Supl 3):S1-S82.
15. Mueller XM, Tinguely F, Tevaearai HT, Revelly J, Chioléro R, Segesser L. Pain pattern and left internal mammary artery grafting. Ann Thorac Surg. 2000;70(6):2045-9.
16. Guizilini S, Gomes WJ, Faresin SM, Bolzan DW, Alves FA, Catani R, et al. Avaliação da função pulmonar em pacientes submetidos à cirurgia de revascularização do miocárdio com e sem circulação extracorpórea. Rev Bras Cir Cardiovasc. 2005;20(3):310-6.
17. Guizilini S, Gomes WJ, Faresin SM, Carvalho ACC, Jaramillo JI, Alves FA, et al. Efeitos do local de inserção do dreno pleural na função pulmonar no pós-operatório de cirurgia revascularização do miocárdio. Rev Bras Cir Cardiovasc. 2004;19(1):47-54.
18. Leguisamo CP, Kalil AKR, Furlani AP. A efetividade de uma proposta fisioterapêutica pré-operatória para cirurgia de revascularização do miocárdio. Rev Bras Cir Cardiovasc. 2005;20(2):134-41.
19. Vasconcelos Filho PO, Carmona MJC, Auler Junior JOCA. Peculiaridades no pós-operatório de cirurgia cardíaca no paciente idoso. Rev Bras Anestesiol. 2004;54(5):707-7.

 All scientific articles published at www.rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbccv.org.br are licensed under a Creative Commons license